Not all surgical meshes are created equal. While gynaecological mesh has rightly attracted controversy due to serious complications in the past, hernia mesh tells a very different story—one of innovation, improved outcomes, and lives changed for the better. It’s important to separate the two, so patients understand that ‘mesh’ isn’t a one-size-fits-all term
In recent years, surgical mesh has been the focus of significant media attention, often highlighting concerns and negative outcomes – particularly in the field of gynaecology. It is understandable that patients may feel uncertain, or even fearful, about whether mesh is a safe or appropriate option. As with many medical devices, however, the reality is more nuanced : surgical mesh can be highly beneficial in the right setting, though it carries risks that must be carefully considered.
Gynaecological Mesh
Importantly, “mesh” is not a single product but a broad category of implants used in different ways. The distinction between gynaecological mesh and hernia mesh is critical. In gynaecology, polypropylene mesh was used for vaginal prolapse, but complications such as mesh erosion, chronic pain and contraction were unfortunately common, sometimes leading to severe, life-altering consequences. These experiences rightly prompted changes in pelvic floor surgery practice.
Hernia Mesh
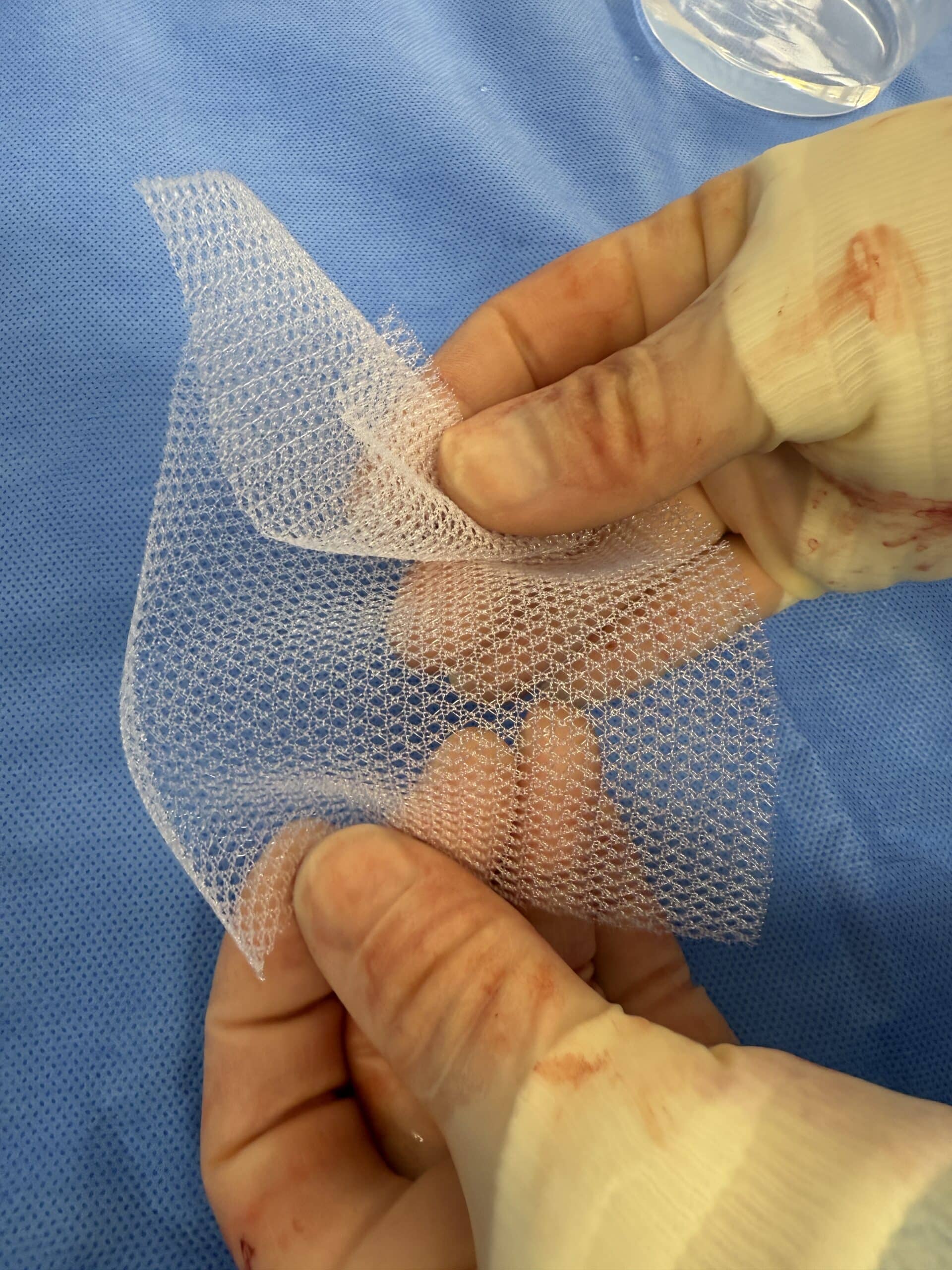
By contrast, the use of mesh in abdominal hernia repair has been far more successful and is supported internationally as the standard of care in most cases. For abdominal hernias, mesh provides reinforcement of weakened tissue, markedly reduces the risk of recurrence and offers long-term durability. While no operation is free of potential complications, the risk profile of abdominal hernia mesh is well-established and is considered acceptable when compared with the significantly higher recurrence risk of tissue-only (suture) repair.
The New Zealand Association of General Surgeons (NZAGS)
The NZAGS reflects this position. They note that mesh is a well-established, safe and effective treatment for both groin and ventral hernias when used appropriately, with serious complications being rare. They also emphasise that the concerns raised around gynaecological mesh should not be conflated with hernia surgery, as the settings, outcomes and risks are quite different.
The key message for patients is that not all mesh is the same and not all uses of mesh carry the same risks. For abdominal hernia repair, mesh remains an effective and important tool to achieve durable outcomes. As surgeons, our role is to provide clear, balanced information on both the benefits and potential risks, so patients can make decisions based on facts rather than fear or headlines.