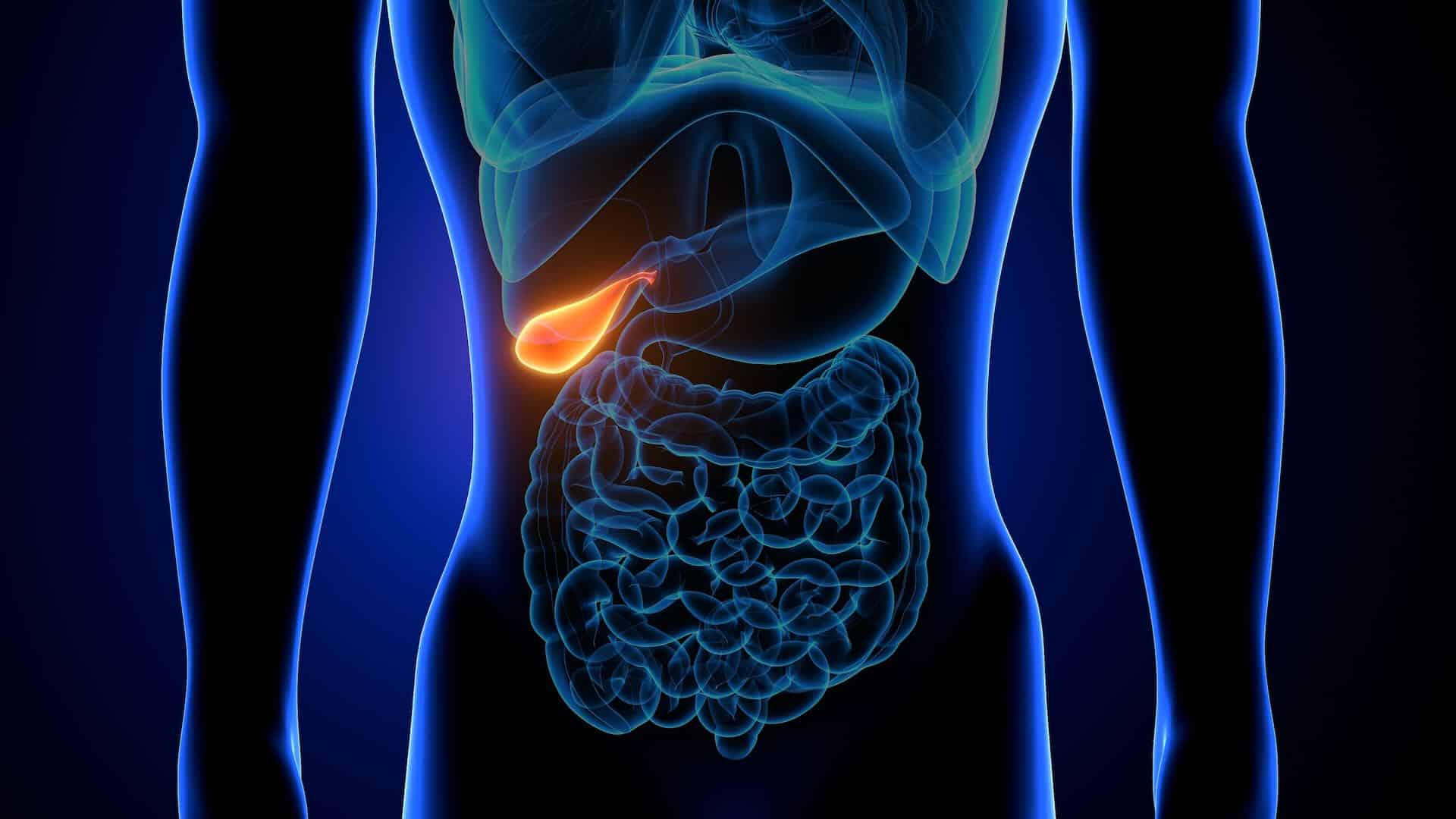
People frequently ask whether removal of the gallbladder, known as cholecystectomy, has any long-term consequence.
The gallbladder plays a role in the digestion of food by storing and concentrating bile, which is released into the small intestine when needed to emulsify fat.
Without a gallbladder, the bile flows directly from the liver into the small intestine and can continue to emulsify fat. Removing the gallbladder therefore doesn’t lead to any loss of digestive function.
The only issue is that the bile secreted into the gut post-cholecystectomy is not as concentrated or readily available as it was when stored in the gallbladder. As a result, some people may experience symptoms following ingestion of large amounts of fatty foods immediately after the surgery, leading to symptoms such as diarrhoea, bloating or cramping, commonly known as post-cholecystectomy syndrome.
Over weeks/months these symptoms usually resolve as the gut accommodates to not having a gallbladder. If one develops intolerance to fatty foods, there are things that you can do to help manage symptoms.
It may be advisable to limit the intake of high-fat foods in the days and weeks following cholecystectomy and then gradually reintroduce them into the diet. One should try and avoid high saturated fat foods and look for foods containing healthy fats, such as those found in avocados, nuts, seeds and olive oil. These fats are generally easier to digest and cause less gut upset.
Eating smaller, more frequent meals throughout the day rather than large meals, with prolonged fasting, can aid digestion and reduce symptoms. In rare cases, one can use bile acid sequestrants to bind to the bile salts which helps alleviate the symptoms.
These can be administered daily for a few months to give the gut time to adapt and usually that helps the gut to accommodate leading to resolution of symptoms.